Blank Tb Test PDF Form
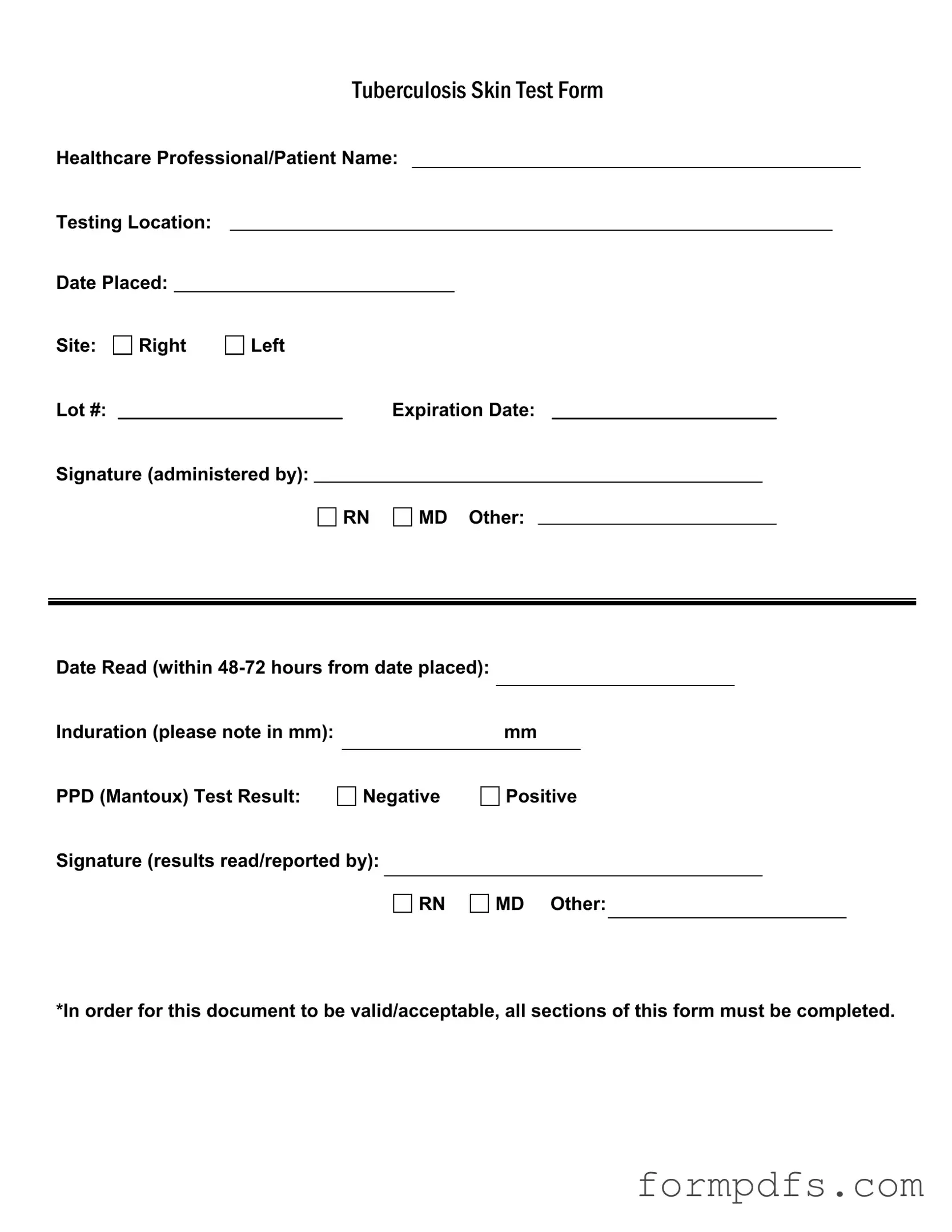
The Tuberculosis (TB) Test form is an essential document used in the healthcare setting to record critical information about the administration and results of the TB skin test, commonly known as the Mantoux test. This form captures vital details such as the names of both the healthcare professional and the patient, ensuring accountability and traceability. It specifies the testing location and includes the date the test was placed, which is crucial for determining the appropriate timeframe for reading the results. The form requires the site of the test to be indicated, whether on the right or left arm, along with the lot number and expiration date of the test materials, ensuring that only valid and safe products are used. The signature of the administering healthcare professional—be it a registered nurse, medical doctor, or another qualified individual—provides verification of the test's administration. After the test is placed, it must be read within 48 to 72 hours, with the results recorded as either negative or positive, and the induration measured in millimeters. The form also requires a signature from the professional who reads and reports the results, reinforcing the importance of accuracy and professionalism in handling such significant health information. To maintain its validity, it is imperative that all sections of this form are completed thoroughly, reflecting the seriousness of TB testing in public health.
More PDF Templates
Medication Administration Record Pdf Fillable - The record indicates changes in medication with a "C," ensuring any adjustments are properly noted.
To facilitate a smooth transaction, it is advisable for both buyers and sellers to utilize a formal document during the sale process. The New York Boat Bill of Sale form can be found at https://smarttemplates.net/fillable-new-york-boat-bill-of-sale/, which offers a comprehensive template to ensure all necessary information is captured accurately, thereby protecting the interests of both parties involved.
How to Setup Direct Deposit - Enjoy peace of mind knowing your funds will be deposited directly.
Documents used along the form
The Tuberculosis (TB) Test form is essential for documenting the results of a TB skin test. However, several other forms and documents often accompany it in healthcare settings. These documents help ensure comprehensive patient care and accurate record-keeping. Below is a list of commonly used forms alongside the TB Test form.
- Patient Medical History Form: This document collects important information about the patient's past medical conditions, surgeries, and family health history. It helps healthcare providers understand the patient's overall health and any potential risks.
- Informed Consent Form: Before administering the TB test, healthcare providers often require patients to sign an informed consent form. This document ensures that patients understand the procedure, its purpose, and any potential risks involved.
- Vehicle/Vessel Transfer Form: For individuals transferring ownership of a vehicle or vessel, the All California Forms provides essential documentation required to ensure compliance with state regulations and proper record-keeping during the transfer process.
- Vaccination Record: This form tracks a patient's vaccination history, including any previous vaccinations against tuberculosis. It provides context for the TB test results and helps healthcare providers make informed decisions.
- Referral Form: If a patient tests positive for TB, a referral form may be necessary for further evaluation or treatment. This document facilitates communication between healthcare providers and specialists.
- Follow-Up Appointment Schedule: After the TB test, patients may need follow-up appointments for further testing or treatment. This document outlines the necessary steps and timelines for continued care.
- Laboratory Test Results: In some cases, additional laboratory tests may be required to confirm TB infection. This document provides detailed results and interpretations from those tests.
- Patient Education Materials: These materials inform patients about tuberculosis, its transmission, prevention, and treatment options. They empower patients to take an active role in their health care.
Having these documents readily available not only streamlines the testing process but also enhances patient safety and care quality. Each form plays a vital role in the overall management of tuberculosis screening and treatment.
Form Breakdown
| Fact Name | Description |
|---|---|
| Form Purpose | The Tuberculosis Skin Test Form is used to document the administration and results of a tuberculosis skin test, commonly known as the PPD test. |
| Healthcare Professional | The form requires the name of the healthcare professional administering the test, which can be a Registered Nurse (RN), Medical Doctor (MD), or other qualified personnel. |
| Testing Location | The form must include the specific location where the test is conducted, ensuring clarity about where the procedure took place. |
| Date Placed | The date when the test is administered must be recorded, as this is crucial for determining the appropriate timeframe for reading the results. |
| Induration Measurement | Induration, measured in millimeters, must be noted on the form. This measurement helps assess the test result's significance. |
| Result Reporting | The test result is indicated as either negative or positive, and the form requires a signature from the healthcare professional who read the results. |
| Completion Requirement | All sections of the form must be completed for it to be valid and acceptable. Incomplete forms may not be recognized. |
| Expiration Date | The form includes a field for the expiration date of the test lot, which is important for ensuring the test's reliability. |
| State-Specific Regulations | In some states, specific laws govern the administration and documentation of tuberculosis tests. For example, California requires adherence to the California Health and Safety Code, Section 121365. |
More About Tb Test
What is the purpose of the TB Test form?
The TB Test form is used to document the administration and results of the Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) test. This form is essential for healthcare professionals to track testing and ensure that all necessary information is recorded accurately for patient safety and follow-up care.
Who is responsible for filling out the TB Test form?
The form should be completed by the healthcare professional who administers the test. This could be a registered nurse (RN), medical doctor (MD), or another qualified individual. It is crucial that the person administering the test provides their signature to validate the document.
What information must be included in the TB Test form?
All sections of the TB Test form must be filled out for it to be considered valid. This includes the patient's name, testing location, date the test was placed, the site of administration (right or left arm), lot number, expiration date of the test, and the signature of the administering healthcare professional. Additionally, the date the test is read and the measurement of induration in millimeters must be recorded.
How soon should the TB Test be read after administration?
The TB Test must be read within 48 to 72 hours after it has been placed. This timeframe is critical for accurately assessing the test result, as the induration, or swelling, can change over time. Reading the test outside this window may lead to inaccurate results.
What do the results of the TB Test indicate?
The TB Test results can be either negative or positive. A negative result typically indicates that the person has not been infected with the TB bacteria. Conversely, a positive result suggests that the person may have been exposed to TB and requires further evaluation, which may include additional testing or a chest X-ray.
What should be done if the TB Test result is positive?
If the test result is positive, it is important to consult a healthcare provider for further evaluation. This may involve additional tests to determine if the TB infection is active or latent. Treatment options will depend on the specific circumstances of the individual’s health and risk factors.
Can the TB Test form be used for multiple patients?
No, the TB Test form is intended for use with a single patient. Each patient must have their own completed form to ensure that their specific information and test results are accurately recorded and easily accessible for future reference.
What happens if the TB Test form is incomplete?
An incomplete TB Test form may be deemed invalid and could lead to complications in patient care. It is essential to ensure that all sections of the form are filled out completely before submitting it. Incomplete forms may not be accepted by healthcare facilities or for employment requirements.
Where should the completed TB Test form be submitted?
The completed TB Test form should be submitted to the appropriate healthcare facility, employer, or organization requiring the test. This could include schools, workplaces, or healthcare providers. Always check with the specific requirements of the institution to ensure compliance.
Tb Test: Usage Steps
Completing the TB Test form is a straightforward process that requires careful attention to detail. Once filled out, this form will serve as an important record of your TB test results. Follow these steps to ensure that all necessary information is accurately recorded.
- Begin by entering the Healthcare Professional/Patient Name at the top of the form.
- Next, fill in the Testing Location where the test is being conducted.
- Record the Date Placed, which is the date when the test was administered.
- Indicate the Site of the test by marking either Right or Left.
- Write down the Lot # associated with the test.
- Fill in the Expiration Date of the test.
- Have the healthcare professional administering the test sign in the Signature (administered by) section, selecting their title: RN, MD, or Other.
- Leave space for the Date Read, which should be filled in within 48-72 hours from the date placed.
- Measure the Induration in millimeters and note it in the designated area.
- Check the result of the PPD (Mantoux) Test and mark either Negative or Positive.
- Finally, have the healthcare professional who reads the results sign in the Signature (results read/reported by) section, again selecting their title: RN, MD, or Other.
Once all sections are completed, review the form for accuracy before submission. This will ensure that your test results are documented correctly and can be easily referenced in the future.