Blank Progress Notes PDF Form
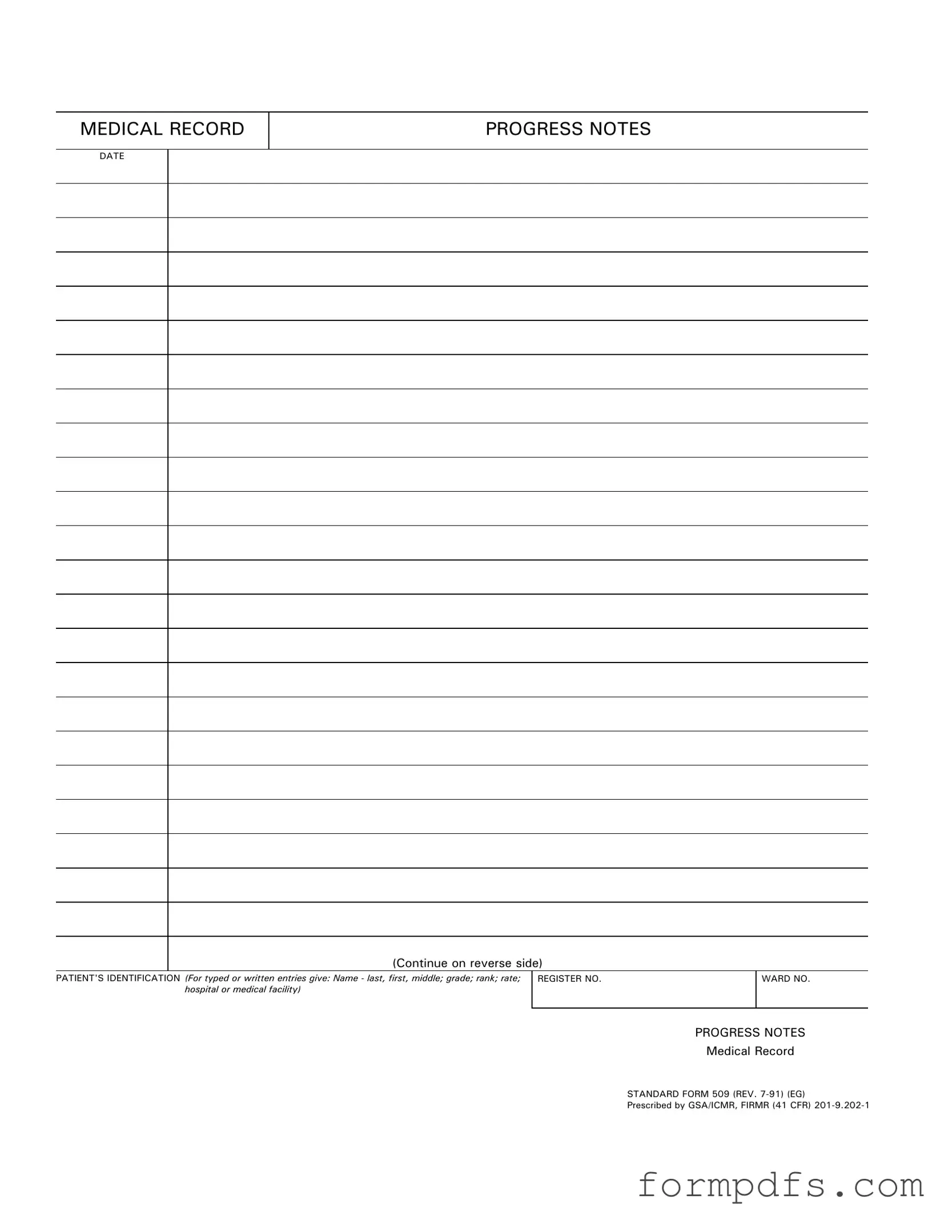
The Progress Notes form plays a crucial role in the documentation of patient care within medical facilities. This standardized form, known as Standard Form 509, captures essential information about a patient's treatment and progress over time. Typically, it includes sections for the patient's identification, such as their name, grade, rank, and hospital or medical facility details. Additionally, the form is designed to record the date of each entry, ensuring that all notes are chronologically organized. By providing a clear and structured way to document observations, treatments, and responses, Progress Notes facilitate effective communication among healthcare providers. They serve not only as a record of care but also as a tool for ongoing assessment and planning. Understanding how to properly fill out and utilize this form is vital for healthcare professionals, as it supports the continuity of care and enhances patient safety. The form's design emphasizes clarity and efficiency, making it an indispensable part of a comprehensive medical record.
More PDF Templates
Shared Well Agreement Template - Emergency procedures for water system failures are described within the contract.
For individuals seeking clarity on the transaction process, understanding the key elements involved in a reliable Arizona bill of sale document is essential. This means being aware of the necessary details that should be included. To assist in completing this process effectively, you can find more information by visiting our resource on the critical Arizona bill of sale guidelines.
Drivers Time Record Sheet - The record helps verify that drivers take required rest periods.
Documents used along the form
The Progress Notes form serves as an essential component in documenting a patient's ongoing treatment and health status. However, it is often accompanied by various other forms and documents that enhance the overall understanding of a patient's care and history. Below is a list of commonly used forms that complement the Progress Notes.
- Patient Intake Form: This document gathers essential information about the patient, including personal details, medical history, and current medications. It is typically filled out during the first visit and helps healthcare providers understand the patient's background.
- Consent for Treatment: Before any medical procedure or treatment, patients are usually required to sign a consent form. This document ensures that patients are informed about the risks and benefits of the treatment they will receive.
- Discharge Summary: Upon a patient's discharge from a medical facility, a discharge summary is created. This document outlines the patient's treatment during their stay, follow-up care instructions, and any medications prescribed for home care.
- Commercial Lease Agreement: Understanding the All California Forms is essential for any business tenant to navigate the terms of leasing commercial property effectively.
- Medication Administration Record (MAR): The MAR is a detailed record that tracks the medications administered to a patient. It includes information such as dosages, administration times, and any reactions observed, ensuring accurate medication management.
- Referral Form: When a healthcare provider determines that a patient requires specialized care, a referral form is issued. This document provides the necessary information to the referred specialist, including the reason for the referral and relevant medical history.
- Insurance Verification Form: This form is used to confirm a patient's insurance coverage and benefits. It is crucial for ensuring that the services provided will be covered and helps prevent unexpected medical bills.
In summary, the Progress Notes form is just one piece of a larger puzzle in the healthcare documentation process. Each of the aforementioned forms plays a vital role in creating a comprehensive picture of a patient's care, ensuring that all aspects of treatment are well-documented and communicated among healthcare providers.
Form Breakdown
| Fact Name | Description |
|---|---|
| Purpose | The Progress Notes form is used to document a patient's ongoing medical care and treatment. |
| Standardization | This form is a standardized document, known as Standard Form 509, ensuring consistency across medical records. |
| Governing Laws | In the U.S., the use of this form is governed by federal regulations including the GSA and ICMR guidelines. |
| Patient Identification | It requires detailed patient identification, including name, grade, rank, and medical facility. |
| Revision Date | The current version of the form was last revised in July 1991. |
| Documentation Continuity | Progress Notes allow healthcare providers to track changes in a patient’s condition over time. |
| Reverse Side Use | Additional notes can be continued on the reverse side of the form if more space is needed. |
| Legal Importance | These notes can serve as legal documentation in cases of disputes regarding patient care. |
More About Progress Notes
What is the purpose of the Progress Notes form?
The Progress Notes form is designed to document a patient's ongoing medical care. It serves as a record of observations, treatments, and any changes in the patient's condition. This documentation is crucial for ensuring continuity of care and for providing healthcare professionals with a clear understanding of the patient's history and treatment plan.
What information is required on the Progress Notes form?
When filling out the Progress Notes form, it is essential to include the patient's identification details. This includes the patient's name (last, first, middle), grade, rank, rate, and the name of the hospital or medical facility. Additionally, the date of the entry must be noted. Accurate and complete information helps maintain the integrity of the medical record.
How should I document observations in the Progress Notes?
Observations should be documented clearly and concisely. Use specific language to describe the patient's condition, any treatments administered, and the patient's response to those treatments. It is important to be objective and factual, avoiding personal opinions. This clarity ensures that other healthcare providers can understand the patient's status at a glance.
Can the Progress Notes form be continued on the reverse side?
Yes, if additional space is needed, you may continue your notes on the reverse side of the Progress Notes form. This allows for comprehensive documentation without the need for multiple forms. Ensure that any continued notes are clearly labeled with the date and any relevant patient identification details.
What should I do if I make an error on the Progress Notes form?
If an error is made, it is important to correct it properly. Do not use correction fluid or erase the mistake. Instead, draw a single line through the error, write the correct information next to it, and initial the correction. This method maintains the integrity of the medical record and provides a clear audit trail of changes.
Progress Notes: Usage Steps
Completing the Progress Notes form is essential for maintaining accurate medical records. Follow these steps carefully to ensure all necessary information is recorded correctly.
- Locate the DATE section at the top of the form and fill in the current date.
- In the PATIENT'S IDENTIFICATION section, provide the patient's name in the format: last name, first name, and middle initial.
- Next, include the patient's grade, rank, and rate as applicable.
- Identify the hospital or medical facility where the patient is being treated.
- Enter the REGISTER NO. and WARD NO. in the designated fields.
- Finally, complete the PROGRESS NOTES section with relevant information about the patient's condition and treatment.
Once the form is filled out, review it for accuracy before submission. This ensures that all necessary details are captured and helps maintain a clear record of the patient's care.