Blank Annual Physical Examination PDF Form
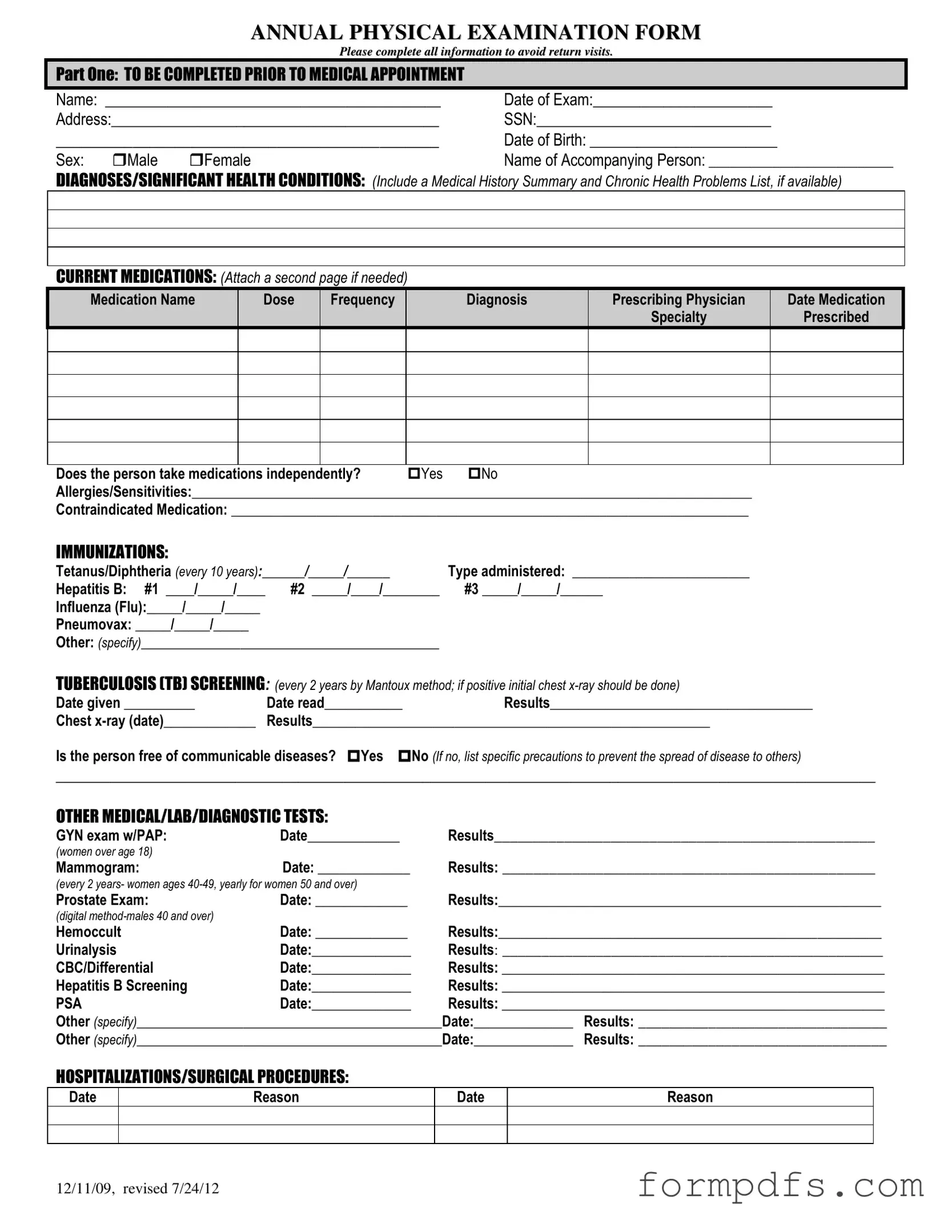
The Annual Physical Examination form serves as a crucial tool in ensuring that individuals receive comprehensive health evaluations. This form encompasses a variety of essential sections that gather pertinent information prior to a medical appointment. It begins with personal details, including the patient's name, date of birth, and contact information, which are vital for accurate record-keeping. The form prompts individuals to disclose any significant health conditions, current medications, and allergies, allowing healthcare providers to tailor their assessments effectively. Immunization history is another key aspect, highlighting the importance of vaccinations like Tetanus, Hepatitis B, and Influenza. Additionally, it addresses tuberculosis screening and outlines necessary medical tests such as mammograms and prostate exams, which are critical for preventive care. The second part of the form focuses on the general physical examination, where vital signs and system evaluations are recorded, ensuring a thorough assessment of the patient’s overall health. By completing this form, patients not only facilitate their own healthcare experience but also contribute to a more effective and personalized approach to medical care.
More PDF Templates
Cg2010 Endorsement Definition - The coverage is limited to specific situations and cannot be applied broadly without reviewing the terms.
The California Homeschool Letter of Intent form serves as a vital communication tool between parents and local school districts, formally indicating a commitment to home education. By submitting this document, parents ensure that their homeschooling practices align with state regulations, paving the way for a tailored educational journey for their children. For more resources, including necessary paperwork, you can explore All California Forms.
Wage and Tax Statement - Social Security wages are listed in Box 3 on the W-2 form.
Documents used along the form
The Annual Physical Examination form is a crucial document that helps healthcare providers assess a patient's overall health. Along with this form, several other documents may be necessary to provide a comprehensive view of a patient's medical history and current health status. Below is a list of additional forms and documents that are often used in conjunction with the Annual Physical Examination form.
- Medical History Form: This form captures a detailed account of a patient’s past medical issues, surgeries, and family health history. It provides essential background information that can influence current treatment plans.
- Medication List: A comprehensive list of all medications a patient is currently taking, including dosages and frequency. This helps healthcare providers avoid potential drug interactions and manage prescriptions effectively.
- Immunization Record: This document outlines a patient’s vaccination history. It is particularly important for tracking required immunizations and ensuring compliance with public health guidelines.
- Motor Vehicle Bill of Sale: This document serves as a vital record for the sale and transfer of a vehicle, ensuring clarity and legality in the transaction. For more details, visit smarttemplates.net/fillable-motor-vehicle-bill-of-sale.
- Referral Form: When a patient needs to see a specialist, this form is used to provide necessary details about the patient's condition and the reason for the referral. It ensures continuity of care between providers.
- Lab Test Orders: This form is used to request specific laboratory tests based on the findings from the Annual Physical Examination. It includes details about the tests needed and any relevant patient information.
- Consent for Treatment: Patients are often required to sign this document to authorize healthcare providers to perform examinations, tests, and treatments. It ensures that patients understand and agree to the procedures being undertaken.
- Patient Information Sheet: This sheet collects essential personal details, including contact information and insurance coverage. It helps streamline the administrative process during medical visits.
- Follow-Up Care Plan: After the examination, a care plan may be created to outline recommended treatments, lifestyle changes, and follow-up appointments. This document is vital for ongoing health management.
These forms and documents play a significant role in ensuring that healthcare providers have the necessary information to deliver effective and personalized care. Properly completing and submitting these documents can enhance the quality of medical services received.
Form Breakdown
| Fact Name | Description |
|---|---|
| Purpose of the Form | The Annual Physical Examination form is designed to collect comprehensive health information from patients prior to their medical appointment, ensuring efficient and effective care. |
| Required Information | Patients must complete personal details, medical history, current medications, and immunization records to avoid delays or return visits. |
| Legal Compliance | In many states, annual physical examinations are governed by health regulations that require healthcare providers to maintain accurate medical records, including patient history and current medications. |
| Screening Recommendations | The form includes recommendations for various screenings, such as vision and hearing tests, ensuring patients receive appropriate preventive care based on age and health status. |
More About Annual Physical Examination
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to collect comprehensive health information before your medical appointment. This information helps healthcare providers assess your health status, identify any significant health conditions, and determine the necessary evaluations or treatments. Completing the form accurately ensures a more efficient visit and can reduce the need for follow-up appointments.
What information do I need to provide on the form?
You will need to provide personal details such as your name, date of birth, address, and Social Security number. Additionally, the form requires a summary of your medical history, current medications, allergies, and any previous hospitalizations or surgeries. You should also list any significant health conditions and provide information about your immunizations and recent medical tests.
How often should I complete this form?
You should complete the Annual Physical Examination form each year before your physical examination. This annual update allows your healthcare provider to track changes in your health over time and make informed decisions about your care. If there are significant changes in your health or medications throughout the year, it’s advisable to update the form before your next appointment.
What happens if I don’t complete the form?
If the form is not completed prior to your appointment, it may result in delays or the need for additional visits. Incomplete information can hinder your healthcare provider's ability to assess your health accurately. To avoid this, take the time to fill out the form thoroughly and bring it with you to your appointment.
Annual Physical Examination: Usage Steps
Completing the Annual Physical Examination form is essential for ensuring that all necessary health information is accurately captured before your medical appointment. This will help streamline your visit and avoid any need for return visits due to incomplete information. Follow these steps to fill out the form properly.
- Personal Information: Fill in your name, date of exam, address, Social Security Number, date of birth, and sex. Include the name of the person accompanying you, if applicable.
- Medical History: Describe any significant health conditions or diagnoses. If you have a medical history summary or a list of chronic health problems, attach it.
- Current Medications: List all medications you are currently taking. For each medication, provide the name, dose, frequency, diagnosis, prescribing physician, and date prescribed. Indicate whether you take medications independently and list any allergies or sensitivities.
- Immunizations: Record the dates and types of immunizations you have received, including Tetanus/Diphtheria, Hepatitis B, Influenza, and Pneumovax.
- Tuberculosis Screening: Note the date the TB test was given and read, along with the results. If applicable, include details about any chest x-rays.
- Other Medical Tests: Document any additional medical, lab, or diagnostic tests you have had, including dates and results for exams like GYN, mammograms, prostate exams, and others.
- Hospitalizations/Surgical Procedures: List any past hospitalizations or surgeries, including the date and reason for each.
- General Physical Examination: Fill in your blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluation of Systems: Indicate whether normal findings were observed for various systems (e.g., eyes, ears, lungs). Provide comments or descriptions as necessary.
- Vision and Hearing Screening: Check whether further evaluation is recommended for vision and hearing, if applicable.
- Additional Comments: Review your medical history summary, note any changes in medications, and provide recommendations for health maintenance, diet, and activity limitations.
- Physician Information: At the end of the form, print your physician's name, and have them sign and date the form. Include their address and phone number.
Once you have filled out the form, review it for completeness and accuracy. Bring the completed form to your appointment to ensure a smooth process and to provide your healthcare provider with all necessary information.