Blank Advance Beneficiary Notice of Non-coverage PDF Form
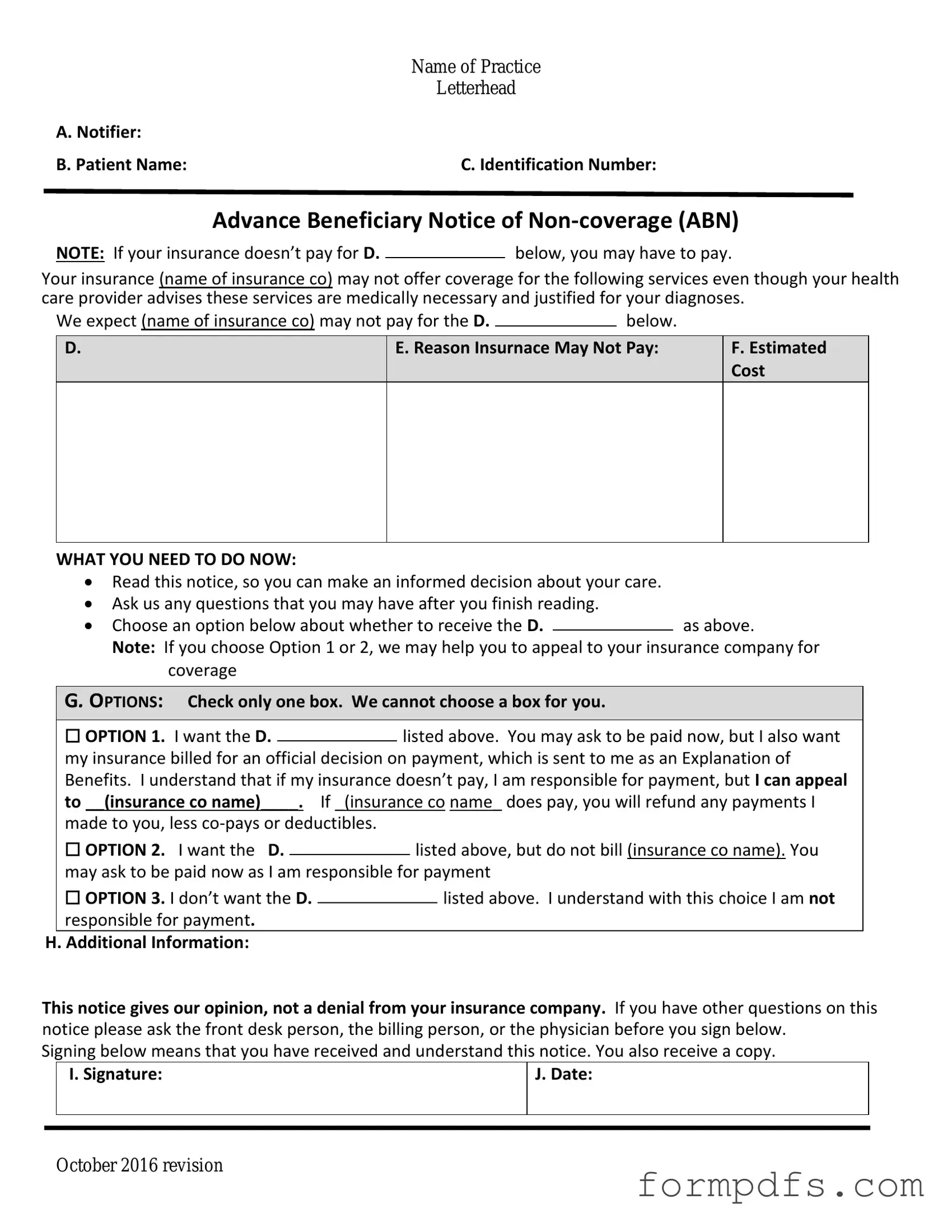
The Advance Beneficiary Notice of Non-coverage (ABN) is a crucial document used in the healthcare system, particularly within Medicare services. This form serves as a notification to beneficiaries that a specific service or item may not be covered by Medicare, allowing patients to make informed decisions regarding their healthcare options. By providing this notice, healthcare providers ensure that patients are aware of their potential financial responsibilities before receiving services. The ABN outlines the reasons for non-coverage, details the estimated costs, and offers beneficiaries the choice to either proceed with the service or forgo it. This form is essential for maintaining transparency between providers and patients, as it helps prevent unexpected medical bills and fosters better communication about coverage limitations. Understanding the ABN is vital for beneficiaries to navigate their healthcare effectively and to understand their rights regarding Medicare coverage.
More PDF Templates
Vaccination Card - This record is not just paperwork; it's a gateway to a healthy life.
Completing the necessary paperwork is essential for couples preparing for marriage, and the Florida Marriage Application Form is a key document in this process. For couples interested in accessing this form, resources such as All Florida Forms can provide the required templates and guidelines. It is important to remember that once the marriage application is submitted, the couple must obtain their marriage license within 60 days and ensure the ceremony takes place in Florida to make the union official.
What Is Form 1040 - Form 1040 requires personal information, including Social Security numbers for the taxpayer and dependents.
Documents used along the form
The Advance Beneficiary Notice of Non-coverage (ABN) is an important document that informs patients about services that may not be covered by Medicare. When working with the ABN, various other forms and documents are often utilized to ensure proper communication and understanding between healthcare providers and patients. Below is a list of related documents that may accompany the ABN.
- Medicare Summary Notice (MSN): This document provides a summary of services billed to Medicare, including what was covered and what the patient may owe.
- Notice of Exclusion from Medicare Benefits (NEMB): This notice explains services that are not covered by Medicare, helping patients understand their financial responsibilities.
- Patient Authorization Form: This form allows healthcare providers to share a patient’s medical information with other parties, such as family members or insurance companies.
- Claim Form (CMS-1500): This is the standard form used by healthcare providers to bill Medicare and other insurers for services rendered.
- Consent for Treatment Form: This document ensures that patients give informed consent before receiving medical treatment or procedures.
- Financial Responsibility Agreement: This agreement outlines the patient's financial obligations regarding services provided, including payment plans if necessary.
- Medicare Enrollment Form: This form is used by individuals to enroll in Medicare, ensuring they receive the benefits they are entitled to.
- Appeal Form: If a claim is denied, this form allows patients to appeal the decision, seeking a review of the coverage determination.
- Authorization for Release of Information: This document permits healthcare providers to release a patient’s medical records to authorized individuals or entities.
- Arizona Lease Agreement Form: For securing your rental arrangements, it’s important to complete the essential Arizona Lease Agreement form requirements for a clear understanding of your obligations.
- Patient Satisfaction Survey: This survey collects feedback from patients regarding their experience with healthcare services, helping providers improve care.
Understanding these documents can help patients navigate their healthcare experiences more effectively. Each form plays a vital role in ensuring transparency and communication between patients and providers, ultimately supporting informed decision-making regarding medical care.
Form Breakdown
| Fact Name | Description |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs Medicare beneficiaries that a service may not be covered. |
| When to Use | Providers must issue an ABN when they believe Medicare will deny payment for a service or item. |
| Beneficiary Rights | Patients have the right to receive the ABN before receiving the service, allowing them to make informed decisions. |
| Signature Requirement | Beneficiaries must sign the ABN to acknowledge their understanding of potential non-coverage. |
| State-Specific Forms | Some states may have specific ABN forms that comply with local regulations. For example, California's ABN follows the California Welfare and Institutions Code. |
| Validity Period | An ABN is valid for the specific service or item listed and must be retained in the patient's file for future reference. |
| Impact on Billing | If a beneficiary signs the ABN and the service is not covered, they may be billed directly for the service. |
More About Advance Beneficiary Notice of Non-coverage
What is the Advance Beneficiary Notice of Non-coverage (ABN)?
The Advance Beneficiary Notice of Non-coverage, commonly known as an ABN, is a form that healthcare providers use to inform Medicare beneficiaries that a service or item may not be covered by Medicare. This notice allows patients to make informed decisions about their healthcare options and potential costs before receiving services that might not be reimbursed by Medicare.
When should I receive an ABN?
You should receive an ABN when your healthcare provider believes that a specific service or item may not be covered by Medicare. This typically happens before the service is provided. The provider must explain why they think coverage is unlikely and provide you with the opportunity to decide whether to proceed with the service or item at your own expense.
What information does the ABN include?
The ABN includes several key pieces of information. It outlines the specific service or item in question, the reason why the provider believes Medicare may not cover it, and the estimated cost you may incur if you choose to proceed. Additionally, the form provides options for you to indicate whether you wish to receive the service despite the potential lack of coverage.
What happens if I don’t sign the ABN?
If you choose not to sign the ABN, your healthcare provider may not provide the service or item in question. In some cases, they may proceed without the ABN, but you could still be responsible for the costs if Medicare denies coverage. Signing the ABN gives you the clarity needed to understand your financial responsibility.
Can I appeal a decision if Medicare denies coverage after I received an ABN?
Yes, you can appeal a decision if Medicare denies coverage for a service for which you received an ABN. The appeal process allows you to challenge the denial and provide additional information or documentation that may support your case. It’s important to follow the specific guidelines provided by Medicare for the appeals process.
Is there a cost associated with services listed on the ABN?
Yes, if you decide to proceed with a service or item after receiving an ABN, you may be responsible for the full cost if Medicare denies coverage. The ABN will typically include an estimated cost, but the actual amount may vary. It’s advisable to discuss any potential costs with your healthcare provider before signing the ABN.
Can I receive an ABN for services covered by Medicare?
Yes, you can receive an ABN for services that are generally covered by Medicare if there is a specific reason the provider believes coverage may not apply in your case. This can happen due to factors such as the frequency of services, the specific diagnosis, or changes in Medicare policy. The ABN ensures that you are aware of the potential for non-coverage even for typically covered services.
Advance Beneficiary Notice of Non-coverage: Usage Steps
Completing the Advance Beneficiary Notice of Non-coverage (ABN) form is a straightforward process. This form is essential for notifying patients about services that may not be covered by Medicare. Follow the steps below to ensure accurate completion.
- Begin by entering the patient's name at the top of the form.
- Fill in the patient's Medicare number, which can be found on their Medicare card.
- Provide the date of the service or the expected date of service in the designated area.
- Clearly describe the service or item that is being provided. Use simple language to ensure understanding.
- Indicate the reason why the service may not be covered by Medicare. Be concise but thorough in your explanation.
- In the next section, check the appropriate box to indicate whether the patient agrees or disagrees with the notice.
- Have the patient sign and date the form to acknowledge receipt of the notice.
- Make a copy of the completed form for your records and provide the original to the patient.
Once the form is filled out, it should be reviewed for accuracy. This ensures that the patient understands their potential financial responsibility for the service. Clear communication is key to avoiding confusion and ensuring compliance with Medicare regulations.