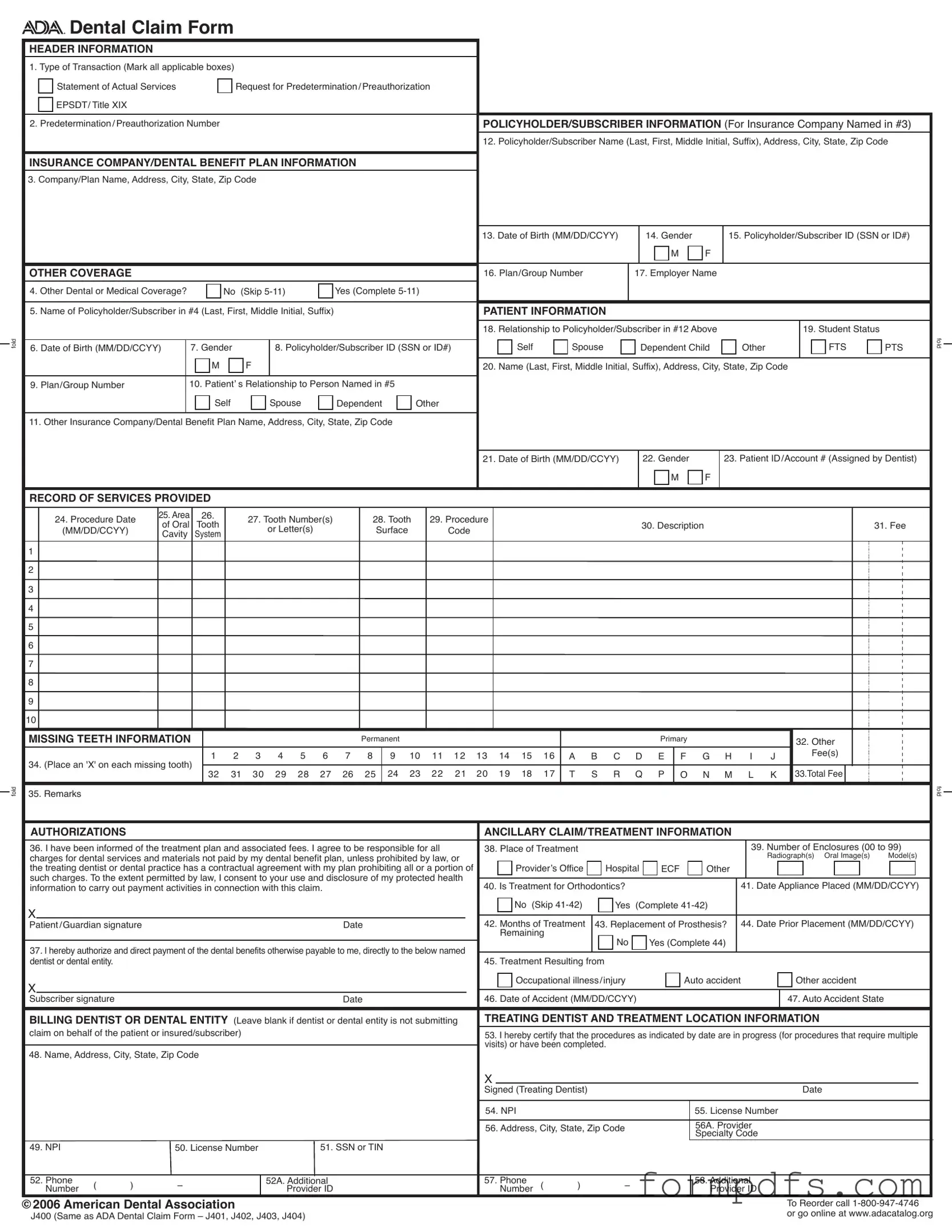
Blank Ada Dental Claim PDF Form
The ADA Dental Claim Form serves as a crucial document in the dental insurance process, ensuring that patients receive the coverage they need for their dental care. This form captures essential information about the transaction type, whether it is a statement of actual services or a request for predetermination. Key sections include details about the policyholder and patient, such as names, addresses, and identification numbers. It also requires information about any other dental or medical coverage the patient may have. The record of services provided is a vital part of the form, detailing the procedures performed, dates, and associated fees. Additionally, it includes sections for authorizations, allowing the dentist to direct payment to themselves for the services rendered. The form ensures that all relevant data is collected, including the treating dentist's information and any necessary attachments, such as radiographs or models. By following the guidelines outlined in the form, dental professionals can facilitate a smoother claims process, ultimately benefiting their patients and ensuring they receive the necessary reimbursements for their services.
More PDF Templates
Shared Well Agreement Template - The process for termination of the agreement is articulated clearly for parties involved.
In addition to the MC-020 form, individuals involved in legal proceedings in California can benefit from accessing a comprehensive collection of documents, guidelines, and instructions necessary for their cases, including resources available through All California Forms. This resource helps ensure that all submissions are completed accurately and efficiently, contributing to a smoother legal process.
Printable Medicare Abn Form 2023 - Providers must give patients enough time to read and sign the notice prior to service delivery.
Documents used along the form
When submitting an ADA Dental Claim Form, several other documents may be required to ensure a smooth claims process. Each of these forms plays a critical role in providing necessary information to the insurance company or dental benefit plan. Below is a list of commonly used documents that accompany the ADA Dental Claim Form.
- Explanation of Benefits (EOB): This document outlines the amount the insurance company has paid for the dental services rendered. It is essential for claims involving coordination of benefits.
- Patient Registration Form: This form collects essential information about the patient, including personal details and insurance information. It helps establish the patient’s eligibility for benefits.
- Authorization for Release of Information: Patients must sign this form to allow their dental provider to share their health information with the insurance company. This is crucial for processing claims.
- Treatment Plan: A detailed outline of the proposed dental procedures, including costs and expected outcomes. This document is often required for preauthorization requests.
- Referral Form: If the patient was referred to a specialist, this form provides information about the referring dentist and the reason for the referral. It can support the claim process.
- Preauthorization Request Form: Used to obtain approval from the insurance company before certain procedures are performed. This helps ensure coverage for the treatment.
- Claim Adjustment Request Form: If there are discrepancies in the claim, this form is used to request adjustments. It provides the insurance company with the necessary details to review the claim.
- Proof of Payment: This document shows that the patient has paid for services upfront. It can help in situations where the insurance company needs to verify payment before processing a claim.
- Articles of Incorporation: To establish a corporation in New York, essential documents such as Articles of Incorporation must be submitted. For more information, visit smarttemplates.net/fillable-new-york-articles-of-incorporation.
- Patient Consent Form: This form confirms that the patient agrees to the treatment and understands the associated costs. It is often required for legal and ethical reasons.
Having these documents ready can significantly streamline the claims process. Ensure that all forms are completed accurately and submitted promptly to avoid delays in reimbursement. Each document serves a purpose in supporting the claim and ensuring that all parties are informed and compliant with necessary regulations.
Form Breakdown
| Fact Name | Details |
|---|---|
| Type of Transaction | The form allows for multiple transaction types including Statement of Actual Services and Request for Predetermination/Preauthorization. |
| Policyholder Information | It requires the policyholder's full name, address, and date of birth. |
| Other Coverage | If there is other dental or medical coverage, additional information must be provided about that coverage. |
| Record of Services | Details of the procedures performed, including dates and fees, must be documented on the form. |
| Authorization for Payment | The form includes a section where the patient authorizes payment to the dental provider directly. |
| Governing Law | State-specific forms may be governed by state insurance laws, which vary by jurisdiction. |
More About Ada Dental Claim
What is the ADA Dental Claim Form used for?
The ADA Dental Claim Form is used to submit claims for dental services to insurance companies or dental benefit plans. It includes essential information about the patient, the policyholder, and the services provided. By filling out this form accurately, dental offices can ensure that claims are processed efficiently and that patients receive the benefits they are entitled to.
How do I fill out the header information on the form?
The header section requires you to indicate the type of transaction, such as whether it’s a statement of actual services or a request for preauthorization. You also need to provide the predetermination number if applicable. Make sure to include the policyholder's name and address, as well as the insurance company's details. This information is crucial for the claim to be directed to the correct payer.
What should I include in the patient information section?
In the patient information section, you need to provide details such as the patient's relationship to the policyholder, their date of birth, and gender. It’s also important to include the patient’s address and any other insurance coverage they may have. This information helps to establish the patient's eligibility for benefits and ensures accurate processing of the claim.
What if the patient has other dental or medical coverage?
If the patient has other dental or medical coverage, you must complete additional sections of the form. This includes providing the name of the policyholder for the other coverage, their relationship to the patient, and details about the other insurance plan. This information is vital for coordinating benefits and ensuring that the claims are processed correctly.
How do I document the services provided on the claim form?
The services provided should be documented in the "Record of Services Provided" section. You will need to include the procedure date, area, tooth number, procedure code, and a description of the services rendered. Additionally, you must list the fees associated with each procedure. Accurate documentation is essential for the claim to be considered valid and for the reimbursement process to begin.
What is the purpose of the authorization section on the form?
The authorization section allows the patient or guardian to consent to the use of their health information for payment activities related to the claim. By signing this section, the patient agrees to be responsible for any charges not covered by their dental benefit plan. This ensures that the dental practice can receive payment directly from the insurance company and clarifies the patient’s financial responsibilities.
Where can I find more information or updates about the ADA Dental Claim Form?
For more information or updates regarding the ADA Dental Claim Form, you can visit the ADA’s website. They provide comprehensive instructions and any changes to the form or its completion guidelines. Staying informed will help ensure that your claims are submitted correctly and processed without delays.
Ada Dental Claim: Usage Steps
Completing the ADA Dental Claim Form is a straightforward process that ensures your dental services are properly billed to your insurance provider. Follow these steps carefully to fill out the form correctly, which will help in expediting the claims process.
- Begin with the header information section. Mark all applicable boxes for the type of transaction at the top of the form.
- Enter the predetermination/preauthorization number if applicable.
- Fill in the policyholder/subscriber information, including their name, address, and contact details.
- Provide the insurance company/dental benefit plan information, including the company name and address.
- Indicate the policyholder/subscriber ID number, along with their date of birth and gender.
- If there is other dental or medical coverage, answer accordingly and fill in the relevant details for the other coverage.
- Complete the patient information section, including the patient's relationship to the policyholder, their date of birth, and gender.
- In the record of services provided section, list the procedure date, area, tooth numbers, and the corresponding fees for each service rendered.
- If applicable, indicate any missing teeth by placing an 'X' on the corresponding teeth in the designated area.
- Fill out the authorizations section, confirming your understanding of the treatment plan and agreeing to be responsible for any charges not covered by the insurance.
- Complete the billing dentist or dental entity information, if necessary, including their name, address, and relevant identification numbers.
- Finally, ensure that the signature and date fields are completed for both the patient or guardian and the treating dentist.
Once the form is completed, review it for accuracy to avoid any delays in processing. Submit the claim to the appropriate insurance company, and keep a copy for your records. This will help ensure that you are reimbursed for the dental services provided.